Reimagining the caries risk assessment: Toward a caries risk conversation
With the advent of caries management by risk assessment (CAMBRA) more than 20 years ago, the past two decades have seen the caries risk assessment develop into a tool that is generally well-understood and -applied across a variety of settings, from private practices to public health clinics. Risk-based care and disease management paradigms promise to cement their use as an indispensable workflow of modern dentistry.
While there are variations between forms—the three most common versions being ADA,1CAMBRA,2 and the AAPD3—one aspect seems to be relatively similar in their implementation. The questions not requiring a dental exam are generally asked exactly as written, leading to a series of yes/no questions for the patient. While useful in generating data points, this is less helpful in engaging patients, understanding their motivations, and guiding them toward behavior changes that promote oral health.
 Figure 1: The caries risk assessment reimagined as a caries risk conversation plus a caries risk examinationIn this article, we propose a framework for helping clinicians ask many of the caries risk assessment questions more effectively, changing the caries risk assessment into a caries risk conversation plus a caries risk examination (figure 1).
Figure 1: The caries risk assessment reimagined as a caries risk conversation plus a caries risk examinationIn this article, we propose a framework for helping clinicians ask many of the caries risk assessment questions more effectively, changing the caries risk assessment into a caries risk conversation plus a caries risk examination (figure 1).
The traditional caries risk assessment
Commonly used caries risk assessments have between 10 and 15 variables not requiring a dental exam that help a clinician understand a patient’s various risk and protective factors for developing dental caries. These variables tend to address patient behaviors, such as oral hygiene routines and care-seeking intervals. A few examples include: “Frequent snacks (>3x daily between meals)” (CAMBRA), “Dental home: established patient of record in a dental office” (ADA), and “Child has brushed daily with fluoride toothpaste” (AAPD).
Note that these questions are not closed-ended per se, but the common use is one that adds “Do you…” or a similar variant to the beginning of the variable being assessed. This includes questions such as: “Do you have snacks more than three times a day?” or “Does your child brush with fluoride toothpaste?” Structured in this fashion, patients are often required to give a yes or no answer for several minutes in succession. Unfortunately, patient activation and engagement does not result from this process, especially when followed by a lecture on what they might be “doing wrong.”
Another outcome is patients telling the clinician what they want to hear. As MacLaughlin and colleagues noted,4 patient responses to even one yes/no question were unreliable due to a fear of upsetting the health-care provider. The end outcome is patient alienation.
So, if the traditional method of completing the caries risk assessment has operational shortcomings, what else can we do—considering that we need the answers both to complete the form and, more importantly, to support, engage, and activate the patient in behavior changes that lead to oral health?
The caries risk conversation
The proposed framework, consistent with others we have published,5 advocates for three major changes in clinician behavior when completing the caries risk assessment: (1) The use of open-ended questions instead of closed-ended questions, (2) fewer, well-structured questions, and (3) minimal or no use of a computer or written checklist when talking with the patient. Let’s explore each of these changes below.
The use of open-ended questions: The use of open-ended questions during a caries risk assessment serves many purposes. First, open-ended questions are naturally more engaging for patients, allowing them to tell their story and describe their oral health journey in their own words. Patients are more likely to consider behavior changes that promote health when they have been heard, and often, when the questions are well-structured, they will come up with solutions to their problems. (Example: “I only brush once a day, but I should probably do it at night too.”)
Second, the use of open-ended questions can create rapport and foster trust between clinician and patient, a demonstrable example that patients are more than the sum total of their oral health data points. Patient-reported experience measures (PREMs) often include questions such as, “How good was the practitioner at really listening?” “How good was the practitioner at being interested in you as a whole person?” and “How good was the practitioner in fully understanding your concerns?” (For an example, see the CARE Measure6). The use of open-ended questions—well-supported from years of research in motivational interviewing—is a logical starting point for improving practitioner outcomes in these areas.
The use of fewer, well-structured questions: When open-ended questions are structured well, the same amount of information can generally be gleaned from fewer questions. This not only makes the process feel less like an inquisition to patients but is helpful for clinicians as well. “What’s your experience at the dentist been like?” allows patients to describe not only the qualitative reality of their past dental encounters (e.g., “I’m scared of needles” is helpful information for clinicians to understand when offering patients treatment options that align with their values and preferences), but frequently also includes information that helps answer multiple questions on the caries risk assessment (e.g., “I’ve been going to the dentist consistently every six months, and I haven’t had any cavities since I was a kid” answers variables pertaining to dental home and recent caries experience/treatment).
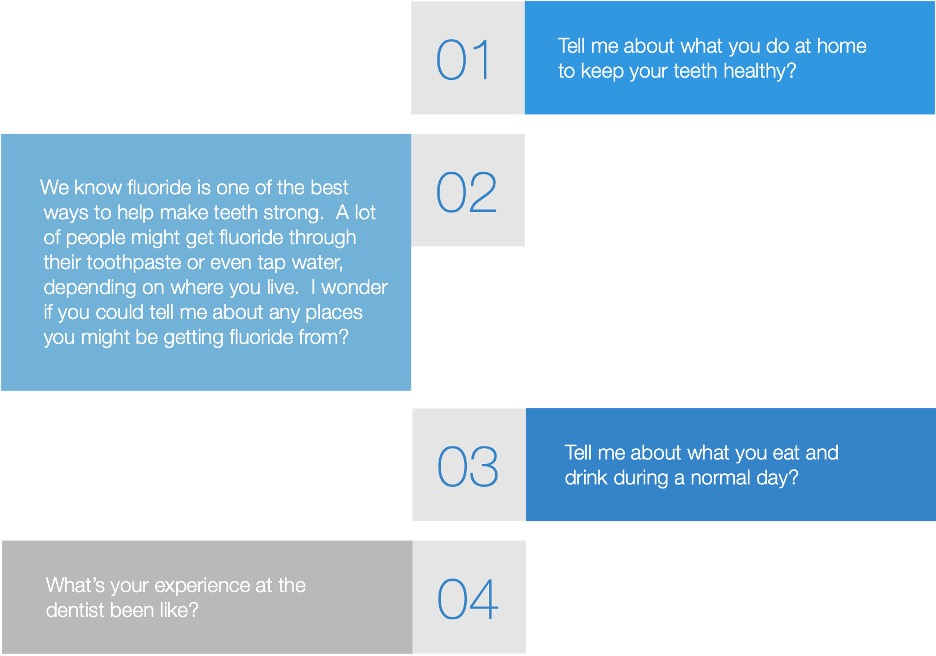 Figure 2: Four open-ended questions for completing the caries risk assessment in an engaging mannerPractically, we have found that most of the information needed to complete the caries risk assessment can be obtained by asking four open-ended questions, with follow-up questions as needed. These four questions (figure 2) are not intended to be normative, but instead they should serve as a starting place for clinician testing, learning, and modification. While we have seen these questions to be useful across a wide variety of settings and with a great number of clinicians, we encourage all clinicians to find their own voices in the conversations to avoid sounding robotic via rote repetition.
Figure 2: Four open-ended questions for completing the caries risk assessment in an engaging mannerPractically, we have found that most of the information needed to complete the caries risk assessment can be obtained by asking four open-ended questions, with follow-up questions as needed. These four questions (figure 2) are not intended to be normative, but instead they should serve as a starting place for clinician testing, learning, and modification. While we have seen these questions to be useful across a wide variety of settings and with a great number of clinicians, we encourage all clinicians to find their own voices in the conversations to avoid sounding robotic via rote repetition.
Minimal or no use of computer or written checklist: A recent study from Haider et al7 at the University of Texas MD Anderson Cancer Center found that clinicians who did not use a computer during a clinical visit were more likely to be seen by patients as more compassionate, displaying more professionalism, and having better communication skills. Given that these are characteristics to which most clinicians aspire, these results, along with a healthy dose of common sense, indicate that clinicians should refrain from using a computer (or a written checklist) when possible.
Considering that the caries risk conversation framework encourages practitioners to use fewer, well-structured questions in an attempt to engage patients while still obtaining useful information, this workflow is an ideal place to meet the patient in a face-to-face dialogue. Most clinicians can return to the computer after the conversation is completed and still input the necessary data in a timely fashion.
Using team-based care to complete the caries risk assessment
A common objection clinicians have to asking open-ended questions of patients is the potential for increasing the time of the encounter. Given the many (and increasing) demands during dental visits, this is not without warrant. To address this concern, we propose that structuring the caries risk assessment as a caries risk conversation plus a caries risk examination delineates clear opportunities for time-saving team-based-care practices.
The caries risk conversation can be completed by any trained office staff and, when done well, often leads to patient-directed goal setting. In the short term, this saves time for practitioners to work to the top of their respective license, and ultimately produces more engaged, healthier patients, which saves time in the long term.
We also believe that helping patients understand why this style is beneficial to their oral health will be seen as a value-added proposition (e.g., “We know you will be most healthy when you’re engaged in your own care, and when we simply collect data points, that tends to be disengaging. So, if it’s OK with you, I’d like to have a conversation with you about your goals for your oral health, current habits that affect your teeth, and, after understanding what your risk is for getting new cavities, how we can work together to reduce that risk and keep your smile healthy and white.”)
In our varied roles, we have seen the caries risk conversation framework applied in a wide array of settings—from national oral health collaboratives to private practice offices, from community health centers to academic institutions. It has been well-received by clinicians and patients alike, promoting relationships and serving as a relatively easy point of entry into more robust patient-centered communication styles and skills (including motivational interviewing, shared decision-making, and goal setting). Ultimately, though a small change, we believe the reimagination of the caries risk assessment workflow is an important shift in mentality, a metaphorical line in the sand as we seek person-centered solutions to existing and necessary workflows in oral health.
Editor’s note: This article first appeared in Through the Loupes newsletter, a publication of the Endeavor Business Media Dental Group. Read more articles and subscribe to Through the Loupes.
References
- Caries Risk Assessment Form (Age >6). American Dental Association. http://www.ada.org/~/media/ADA/Science%20and%20Research/Files/topic_caries_over6.ashx
- Bernie KM. CAMBRA: Caries Management by Risk Assessment. March 1, 2011. DentistryIQ. https://www.dentistryiq.com/practice-management/industry/article/16356688/cambra-caries-management-by-risk-assessment
- American Academy of Pediatric Dentistry. Caries-risk assessment and management for infants, children, and adolescents. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry; 2020:243-247. https://www.aapd.org/media/Policies_Guidelines/BP_CariesRiskAssessment.pdf
- MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging. 2005;22(3):231-255. doi:10.2165/00002512-200522030-00005
- Allen M, Brown C. Five essentials for patient-centered communication during synchronous teledentistry. BDJ In Pract. 2020;33(7):23. doi:10.1038/s41404-020-0447-z
- Welcome to the CARE Measure website. Care Measure. http://www.caremeasure.org/
- Haider A, Tanco K, Epner M, et al. Physicians’ compassion, communication skills, and professionalism with and without physicians’ use of an examination room computer: a randomized clinical trial. JAMA Oncol. 2018;4(6):879-881. doi:10.1001/jamaoncol.2018.0343
 Matthew Allen, DDS, is the CEO and cofounder of DifferentKind. He has spent his career making dental care more human. Dr. Allen is the only US-based dentist member of MINT, the Motivational Interviewing Network of Trainers, and has championed this person-centered communication style as a sought-after consultant, author, speaker, and advocate. He remains active in clinical practice at a nationally recognized community health center in Denver, where he was previously the dental director. He also serves as part-time volunteer faculty at the University of Colorado School of Dental Medicine.
Matthew Allen, DDS, is the CEO and cofounder of DifferentKind. He has spent his career making dental care more human. Dr. Allen is the only US-based dentist member of MINT, the Motivational Interviewing Network of Trainers, and has championed this person-centered communication style as a sought-after consultant, author, speaker, and advocate. He remains active in clinical practice at a nationally recognized community health center in Denver, where he was previously the dental director. He also serves as part-time volunteer faculty at the University of Colorado School of Dental Medicine.
 Carolyn Brown, DDS, MEd, is the COO and cofounder of DifferentKind. She is a health-care change agent, employing operational, analytic, and deep industry knowledge as key components in a consulting practice spanning more than 10 years. Dr. Brown is a veteran subject matter expert in teledentistry, value-based care, medical-dental integration, dental benefits, dental diagnostic coding, health workforce, and health-care transformation. She brings her analytic focus from her corporate and academic backgrounds.
Carolyn Brown, DDS, MEd, is the COO and cofounder of DifferentKind. She is a health-care change agent, employing operational, analytic, and deep industry knowledge as key components in a consulting practice spanning more than 10 years. Dr. Brown is a veteran subject matter expert in teledentistry, value-based care, medical-dental integration, dental benefits, dental diagnostic coding, health workforce, and health-care transformation. She brings her analytic focus from her corporate and academic backgrounds.
